Shaving Routine and Preoperative Surgical Procedures
It is a well-known fact that surgical site infection (SSI) is a condition during which the bacteria sphere and damage the wound after the operation because of the ineffectiveness of mechanism of virulence prevention. Therefore, SSI is considered to be the most frequently occurred infection of nosocomial type, which is predetermined by different factors such as skin preparation, anemia, operative period, and systemic disease. Hence, it is essential to review all possible types of prevention mechanism aimed at reducing the percentage of infection spread into the post-operative wound. It has been reported that the need for routine shaving of a surgical site is under the question because it does not contribute to the reduction of infection after the surgery.
Hence, the purpose of the paper is to review the studies which provide different approaches to reducing the number of viruses and microbes in a postoperative period as well as to introduce alternative ways for minimizing the outcomes of the surgery.
Infection after the Surgery: Healthcare Problem
Surgical site infection is considered to be the most serious problem which undergoes multiple studies and investigations. According to the study conducted by Sasi, Sistla, Sistla, Karthikeyan, Mahalakshmy, and Vikayaghavan (2015), nearly 66 % of the surgical site infections occur as a result of Staphylococcus aureus, which is predetermined by Methicillin-resistant Staphylococcus aureus (MRSA). The attention should also be paid to the analysis of diverse risk factors related to MRSA carriers. Additionally, Itany and Hawn (2013) have underscored the fact that surgical site infection rate is also among the highest ones, particularly among patients who undergo colorectal surgery. It should be stressed that contamination is regarded as the major risk factors, which is also attributed to the patient’s specific flora. At this point, preoperative skin preparation is one of the most important procedures aimed at minimizing the occurrence of surgical site infections, and it should involve the interventions that would decrease the influence of endogenous fiber on the site. There are numerous methods for skin preparations discussed in the research studies such as hair removal by razor, epilator, or cream depilation or no hair removal. These aspects should be discussed in order to understand which method seems to be the most effective one.
Significance of the Problem
It should be acknowledged that shaving has long been the routine procedure for operation preparation. Recently, the role of shaving has been reconsidered and put under doubt. In the studies by Yang and Cheng (2014), the attention has been paid to the need for shaving before craniotomy surgery. Furthermore, the authors have discussed the psychological influence of shaving, one of the major underpinning for anxiety before the surgery, on the patients. The results of the study have revealed that shaving is not always the obligatory condition for reducing the probability of infection emergence after the surgical operation. The significance of the problem is underlined because of the previously established rules of surgical procedures in the light of the growing concern for the spread of nosocomial infections. The complications could even lead to delayed wound healing, revision surgery, or abuse of antiseptics and antibiotics. Increased stay at hospitals has also negative influence on both patients and costs undergone by hospitals. Therefore, proper skin preparation and the development of new methods of infection reduction are on the current agenda to reduce the outcomes of the surgery as well as to define what factors affect the minimization of Staphylococcus aureus appearance (Harrop, Syliaras, Ooi, Radcliff, Vaccaro, & Chengyuan, 2012).
The problem can be solved through synthesizing the available research practices and evidence-based analysis.
Current Practices Related to the Problem
In fact, there are many research practices which put hair removal routine under the question because of the absence of its rationale. Furthermore, some of the research studies state that hair removal can be even more dangerous in terms of the probability of emergence of infection after the surgery. To enlarge on the issue, Jose and Bignon (2013) discuss the preoperative preparation for surgery to withdraw the idea that shaving is an important routine for ensuring cleanness. The review of literature has investigated the connection between preoperative shaving and surgical site infection. The purpose of the review is to define the most important practice of hair removal to minimize the infection in case when hair removal is essential, as well as to apply some new evidence for nursing practice. In response to these studies, Lefebvre, Saliou, Lucet, Mimoz, Keita-Perse, and Aho-Glele (2015) have also presented the meta-analysis of 19 randomized controlled trials to define that there are no tangible advantages of depilation and shaving for preventing infections. Furthermore, shaving creates higher percentage of infection occurrence during and after surgery. Hence, the effectiveness of both depilation and shaving are identical.
The in-depth study conducted by Kshirsagar, Patil, Nangare, and Agarwal (2013) has revealed the compared importance of hair removal before the surgery in all kinds of wound. The results have revealed about 2 % probability of infection among all types in comparison with no hair removal procedure. In case with preoperative shaving, the average percentage was about 6% of infection. The general wound rate amounted to 2.38 %, while infection rate for shaving with razor equaled 8.2 %. Additionally, it has been discovered that the infection rate is higher in case of dirty wound. Finally, the authors have concluded that the importance of hair removal and its influence on SSI had been higher as compared with no hair removal. Therefore, the latter method is much more effective.
Influence of the Problem on Organization’s Cultural Background
Certainly, some of the preoperative procedures have been tested to provide the results, and there is still the range of important conditions when shaving is culturally and traditionally predetermined. As such, Basevi and Lavender (2014) have introduced their view on the role of shaving. Specifically, the authors have explained that “although a significant difference was found in the number of women who had colonized Gram-negative bacteria in favour of those who had been shaved; when combined with Gram-positive bacteria, no differences were found” (Basevi & Lavender, 2014, p. 14). An extensive study has been introduced to define the advantages and disadvantages of routine shaving before child delivery. The results of the study could be applied to various birth environments. Nonetheless, the cultural circumstances still play crucial role in understanding the ethicality of the procedures and explanation to the patients.
The cultural environments could also be under the questions because physicians with diverse background rely on their own experience and knowledge while conducting operations. In response to this fact, Rasouli and Kopel (2016) have tried to break the stereotypes and expand the views about surgical site infections through the use of medicines and other pre-operative procedures. They have explored the influence of vancomycin power for reducing the probability of SSIs after spinal and cranial surgery. However, the use of method during the deep brain stimulation surgery is under the question. Therefore, the major task of the research was to explore the author’s experience of the use of power to prevent infection spread in a postoperative period.
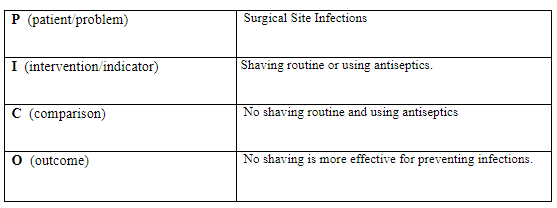
Table 1 PICO Questions
Number and Types of Articles Available for the Search
The articles presented for the research studies introduce the evidence regarding the need to reconsider shaving, depilation, and other types of hair removal as the obligatory condition for preoperative preparation. The evidence also shows the results of the study proving that no hair removal is even more effective and less dangerous for the spread of the infection during and after the surgery.
Recommended Practice Change Addressing the PICO Questions
The majority of the studies evaluated and reviewed have revealed that no hair removal is much more effective. Therefore, the assessment of the evidence, review and the related overview of literature prove the risk of shaving and depilation providing a rationale for reconsidering preoperative practices and introducing new training programs for the hospitals and surgical departments. What is more important, it can unveil new spheres for research such as the analysis of new method of surgery requiring no cuttings (laser surgery) and minimal human interventions, which can maximize the effect and decrease the probability of infection emergence. Additionally, the patients’ specific flora should be studied to understand whether it affects the rate of infection emergence during and after the surgery.
Apart from the introduction of no hair removal, the physicians and nurses should enter new training course of isolation of patients, new hygiene procedures, and the development of new antibiotics, which could eliminate all dangerous viruses and bacteria. Apparently, the resistance to introduce new method of surgery is predetermined at the level of risk of leaving hair near the after-wound surgery site, which is the level of comfortableness and safety as well.
Process for Implementing the Recommendations
Three Key Stakeholders in the Decision to Implement the Recommendation
No hair removal method could be introduced to three major stakeholders, which are physicians, administrators, and patients. All the stakeholders must be notified about new interventions and shifts in surgical procedures. Both physicians and nurses should attend new lectures and training programs where they can learn about new research practices and experiments that prove the effectiveness and rationale for the new method. Further, the managers should invest into the development of new methods and training programs while providing the nurses and physicians with all necessary materials, medicines, and equipment.
The schedule should also be introduced for the stakeholders to understand the deadline for reestablishment and reconsideration of the mechanisms of the surgery procedures. After the stakeholders go through the theoretical course and take part into the test operations, they should also be assessed in terms of comprehending new materials.
The analysis of such materials must be introduced through the development of opportunities for further clarification of methods.
Specific Barriers to Applying the Evidence to Practice Changes in the Nursing Setting
There is a number of barriers and problems which can be encountered by the stakeholders, such as availability of previous practices and stereotyped views on the process of surgery. The latter is the most complicated challenge which prevents the nurses from realizing the value of the innovation. The reluctance to accept something new could also be among the changes.
Further, the managers could be reluctant to introduce such practices because of the absence of additional costs for new training programs as well as for the time and staff that would use training courses.
Two Strategies for Overcoming the Barriers
First of all, the barriers could be overcome with two major strategies – change management and cost-effectiveness motivation. To enlarge on the issue, change management is essential for the personnel to get an idea of the new method. The task of the manager is to provide evidence and explanation of the effectiveness of new methods as well as to introduce facts and evidence regarding negative outcomes and additional expenses for the materials used during preoperative shaving. Second, the cost-effectiveness motivation is more important for the managers who can be reluctant to spend additional time and cost for implementing new program and strategic framework during the surgery. In such a way, they will be able to provide new methods and schemes which could compensate previous expenses.
The change management can contribute to the shifts in behavioral trends, beliefs and perceptions, as well as provide a hospital with competitive advantage over other organizations, hence increasing the quality of healthcare delivery and minimizing the complications. In such a manner, behavioral patterns could be among the priorities for the healthcare administrator. The manager could also organize general meetings for the physicians to discuss the problem and provide better solutions. They could also be motivated for further research in the field as well as for conducting new methods in the sphere of nursing. Such an approach can become a win-win solution for all the stakeholders involved into the program evaluation. The program outcomes could be published in journals for the patient to be persuaded in the results and in the effectiveness of new approaches.
One Indicator to Measure the Outcome Related to the Recommendation
In order to measure the outcome, the program results will be tested and evaluated with the operations conducted with the use of new methods. The operations will be promoted in terms of evidence-based results and empirical studies so that to persuade the patients that these operations are safe and bring in no risk for the health and life. Besides, new types of preoperative procedures are less time-consuming, which is especially important during the cases when time decides the chances for survival. What is more important, the indicator can also shorten the time of the surgery while increasing the percentage of completed surgeries. The problem of surgical site infection could be solved more efficiently.